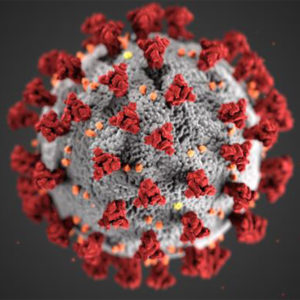
Healthy people volunteering to be infected with SARS-CoV-2, in order to help scientists better understand how to tackle the virus, should receive payment—if it is determined that these studies are otherwise ethical to proceed.
Those are the findings of a new peer-reviewed study published in the American Journal of Bioethics, which has assessed the ethics of paying participants to take part in human infection challenge studies (HICS).
Over the past few months there has been vast media coverage and discussion about the first COVID-19 HICS in the world, planned to begin in the United Kingdom (UK) later this year. This type of study can be particularly valuable for testing vaccines and can speed up the development of new vaccines.
Using HICS for a disease that can be fatal and currently lacks a cure is ethically controversial. Part of that controversy has to do with whether participants should be paid for such a risky endeavor and how payment might affect their consent.
Among the advocates of pursuing COVID-19 challenge trials is the organization, 1Day Sooner, which sponsored the report on which the new study is based, seeking an independent assessment of whether and how much people should get paid to take part in challenge trials.
The international research team from the UK, United States, and Canada does not necessarily endorse the use of HICS for COVID-19, but if HICS proceed, the team’s findings reflect that not only should participants be paid, the payment should be “substantial.”
The research team—including experts in bioethics, economics, science, medicine, and law, as well as two individuals expressing interest in participating in SARS-CoV-2 HICS—created a framework for scientists to follow in order to ethically assess payments for people taking part in HICS. They also looked at payment in similar studies, but noted the difficulty of finding this information.
“Our work was spurred by concerns that payment for SARS-CoV-2 HICS might require a novel ethical framework, which we ultimately determined to be unfounded,” states lead author Holly Fernandez Lynch, an assistant professor of medical ethics with the Perelman School of Medicine at the University of Pennsylvania. “Payment for HICS participation should be treated like payment in other clinical studies involving healthy participants. High offers of payment are sometimes met with scrutiny and concern, but it can be ethically appropriate to offer substantial payment for research participation, and we have to consider that low payment also raises significant ethical concerns.”
Lynch adds that SARS-CoV-2 HICS should not be allowed to proceed in any setting in which adequate provisions have not been made for compensating research-related harms, as well as other efforts to minimize risk and promote social value.
“Our hope going forward is that our analysis will serve both to ease concerns about payment in these studies, should they proceed, and to advance the broader project of ensuring ethical payment to participants in all clinical research,” Lynch says.
Edited by Gary Cramer