Clinical Researcher—April 2022 (Volume 36, Issue 2)
PEER REVIEWED
Preethi Sriram, DHSc, MSN, BSN
Many aspects of the current state of public education and healthcare in America reflect upon the dark history of race relations in the country, in that lingering practices in these arenas have been constructed from a time of apartheid and discrimination that carries its impacts into the modern day.{1} Some of the tragedies found in the history of race relations as it pertains to medical research and healthcare are well known, such as the government-backed Tuskegee syphilis studies focused on the long-term effects of syphilis on Black American men even after an effective cure, penicillin, became available.{2} From this notorious study came about the Belmont Report principles of respect for persons, beneficence, and justice that form the ethical backbone of the modern-day clinical research guidelines.{3}
While the Tuskegee syphilis study and other egregious examples of unethical medical experimentation are often cited as reasons for minority distrust of the medical community, there are less well-known incidences of concepts that have been created in the past 150 years that are still being utilized in healthcare for diagnoses and treatment within a present-day context that need to be reexamined. This paper will explore these concepts with special attention paid to the topics of body mass index (BMI), acute kidney injury (AKI), the spirometer medical device, and the advent of therapies targeted toward specific racial groups.
Body Mass Index (BMI)
Achea Redd, a Black woman, noted that when she would attend her yearly checkups and discuss her fear that she may have an eating disorder, the physicians dismissed her worries, as her BMI did not reflect this possibility. She was later diagnosed by her therapist as having atypical anorexia, yet her insurance would not cover her treatment because of her BMI, and she paid $800 monthly out of pocket to get the specific healthcare guidance she needed.{4}
The concept of BMI is well known by name in healthcare and amongst laymen. This is an index that can be utilized as a benchmark for determining risk for other health conditions. The BMI is calculated using the individual’s height and weight to give an estimate of body fat for both genders and all ages.{5} Figure 1 shows how this is calculated per the height and weight of any given adult individual to reach a categorization of Normal, Overweight, Obese, or Extreme Obesity. This is often used in clinical trials to exclude a patient, as it could imply other underlying health conditions.
Figure 1: Body Mass Index Table
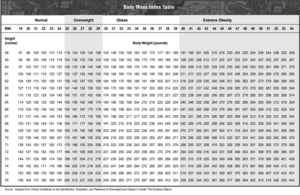
Source: https://www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmi_tbl.pdf
Many though are not aware of the origins of the BMI index, and that it was created in the 1830s by a Belgian man, Lambert Adolphe Jacques Quetelet.{6} This index was created using European men to measure weight and Quetelet noted that it was not supposed to be applied on an individual basis, but as a population level tool. This Quetelet Index was introduced after nearly 140 years in 1972 by a physiologist, Ancel Keys. Sabrina String, an assistant professor at University of California, Irvine, notes that it was created using mostly white males, and that females and other groups had not been included in the analysis when creating the index; accordingly, is not a tool that should be utilized in health outcomes.{7} Thus, the tool is flawed as it does not take gender and other backgrounds into account, nor does into take age into account.
While BMI is not the only marker for health, and there are many different variables that need to be considered when working with an individual, when this index is still utilized inappropriately or in a flawed way, it has consequences—as with the case of Achea Redd. Redd’s healthcare treatment was delayed by her provider as the index was not reflecting the reality that she was suffering from an eating disorder, and even when later diagnosed, insurance would not cover her treatment since she did not meet the predetermined numbers.{4}
Acute Kidney Injury (AKI)
Cases of chronic kidney disease (CKD) and end-stage kidney disease (ESKD) are noted as dramatic examples of race-based health disparities in the U.S. Laster, et al. cite that African Americans experience some of the highest rates of ESKD compared to other ethnic groups.{8} With this information, it would thus seem intuitive that diagnoses and treatment should occur earlier, and the healthcare providers would be vigilant with regards to these data, yet ironically, it seems the opposite when looking from the angle of the formula for diagnosing acute kidney injury (AKI).
AKI is common amongst critically ill patients and can foreshadow a significant impact to CKD, cardiovascular disease, and overall mortality.{9} With regards to AKI, as it is difficult to measure the function of the kidney directly, equations were developed by researchers to determine the estimated glomerular filtration rate (eGFR) using the serum creatinine level.{10} Table 1 shows the normal creatinine levels with categories by age, race, and gender.
Table 1: Estimated Baseline Creatinine
| Age (Years) | Black Males (mg/dl) (mmol/L) | Other Males (mgl/dl) (mmol/L) | Black females (mg/dl) (mmol/L) | Other Females (mg/dl) (mmol/L) |
| 20-24 | 1.5 (133) | 1.3 (115) | 1.2 (106) | 1.0 (88) |
| 25-29 | 1.5 (133) | 1.2 (106) | 1.1 (97) | 1.0 (88) |
| 30-39 | 1.4 (124) | 1.2 (106) | 1.1 (97) | 0.9 (80) |
| 40-54 | 1.3 (115) | 1.1 (97) | 1.0 (88) | 0.9 (80) |
| 55-65 | 1.3 (115) | 1.1 (97) | 1.0 (88) | 0.8 (71)
|
| >65 | 1.2 (106) | 1.0 (88) | 0.9 (80) | 0.8 (71) |
Source: Bellomo R, Ronco C, Kellum, JA, Mehta RL, Palevsky P. 2004. Acute renal failure—definition, outcome measures, animal models, fluid therapy, and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Critical Care 8(4):R204–12. https://doi.org/10.1186/cc2872
The normal levels used as a reference for diagnosing AKI results in higher reported values in anyone identified as Black, and the justification given by the developers of the measurement is that there is a higher serum creatinine amongst Black people versus White people.{10}
While the measure of creatinine may not be the only criteria with regards to determining AKI, it is one of the parameters that is relatively easy when taking into consideration that creatinine values can be determined from blood work when the individual is in the clinic, and thus, the value of creatinine can be very misleading, especially if it is only looked at by itself. Someone with a creatinine value that may be “normal” due to being categorized by a certain race, may actually be overlooked for further care because the value itself may not “flag” during a routine visit. Vyas, et al. cite that the adjustments in the formula with consideration to race may impact the care that those identified as Black patients may receive, may delay counsel for specialist care, and may lead to worse outcomes.{10}
The equation itself seems outdated in that it splits the population between Black and non-Black, though the concept of being Black has more of a social role than a biological one. Bichell and Anthony show just how regressive the concept of using a Black/non-Black equation is with the case where Glenda V. Roberts, whose genetic ancestry shows at least 48% from non-African countries and 25% Native American, could be identified as Black due to social impacts of American culture. The authors note that the race factor does not work as well for Black Europeans or those in West Africa, and that Australian researchers found that the measure also led them overestimate the function of the kidney in native Australians.{11}
Thus, depending on self-identification, as well as judgement/stereotyping of the healthcare provider to categorize the individual as Black or non-Black, an individual is likely to receive different answers about his or her staging of AKI. The type of treatment and care given may be lacking if it is estimated that persons are healthier than they really are and, in fact, are sicker than the formula reflects.
Spirometer
In the past century, the use of spirometers has spread worldwide for the identification and treatment of various respiratory diseases, in both primary care and specialist settings. The spirometer has a correction factor for race—as self-identified by the patient or determined by the judgement of the healthcare provider—programmed by the manufacturer and difficult to deactivate.{12} Figure 2 shows a calculator from the National Institute for Occupational Safety and Health that considers the race of the individual when calculating the spirometry reference.
Interestingly, the race correction that is utilized today has roots in a very racist period of history in America of the 1800s, when Samuel Cartwright, a physician and slaveholder, deemed that enslaved Blacks had lower pulmonary function than Whites and utilized this “finding” to promote the idea that forced labor was good for them.{13} This philosophy was utilized to justify slavery as beneficial—even necessary—in terms of helping the physical condition of enslaved Blacks, yet it did not look into social reasons as to why they may have had lower pulmonary function (i.e., working in environments that may have impacted the lungs, the strains of forced labor, undiagnosed conditions, etc.).
Figure 2: Spirometry Reference Value Calculator
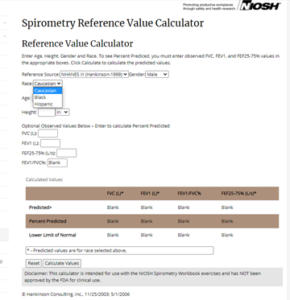
Source: https://www.cdc.gov/niosh/topics/spirometry/refcalculator.html
Healthcare providers may not even be aware of these race corrections programmed into the modern-day spirometer, nor aware of its history, and this ignorance can lead to real consequences. For instance, providers may miss a diagnosis if lower limits are considered normal for the reference population. The spirometer is used to measure forced expiratory volume and this can influence the treatment plans. For example, patients with COVID-19 pneumonia resulting in pulmonary fibrosis may require pulmonary rehabilitation, including breathing exercises and continual monitoring, but this might not be undertaken if the adjustment factor is race programmed and thus leads to an incorrect diagnosis.{14}
This is the reason behind Anderson, et al. urging healthcare providers to be aware of the disparities that may be intensified amongst the racial groups by using a correction for race, and in recent times, particularly considering the pandemic.
Race, Genetics, and the New Frontier
“Race” can have various meanings, but starting in the 18th century, the concept of race was conceived as a biological construct and the archaic categorizations no longer holds scientific merit. Race is currently seen as a social construct—at least, from a scientific viewpoint.{15} Yet, the concepts of race and ethnicity are still being included in medicine and treatment and have very real implications in medicine and healthcare.
Washington notes a certain drug—developed in the late 1990s and originally targeting the general population—was first rejected by the U.S Food and Drug Administration (FDA). This drug was not approved until 2005, only after its developer said that, based on a retrospective data analysis, the drug’s mechanism of action was potentially of benefit against a genetic anomaly that makes African Africans susceptible to congestive heart failure. Although the company had created a perception that the drug worked distinctly in African Americans, this relied on outdated data regarding how many African Americans in a certain age range died from the condition versus Whites—and discounted a variety of nongenetic factors at play in the difference in death rates between the races. In any event, marketing for the product notes it as the only drug indicated for heart failure for those who self-identify as African American, making it seem that there is a distinctive pathophysiological difference between African Americans and other populations with regard to presentation of congestive heart failure. The validity of that claim is spurious, given the data used.{2}
Further, “scientific” terminology used to define who is African American versus White has changed throughout American history. There may be people who are of mixed ancestry, or adopted, or who may appear at first to fall under the societal construct of one paradigm for a certain race, yet in truth fall outside it. If a drug can only be prescribed based on self-identification of one’s race, this raises social quandaries about who is “allowed” to self-identify as belonging to one group or another. For example, should individuals be required to take a genetic test to back up any claims of self-identification for a particular race?
The genetic frontier of personalized ancestry testing is here and brings with it more recent ethical questions. While there are those who recommend using personalized genetic testing to help bridge the gap between healthcare and genetics,{16} the very science of testing ancestry seems to be somewhat murky in that the baseline set of samples is created from a sample population of modern individuals selected with the idea that they are “pure,” or not mixed. Blell and Hunter cite how the concept of a population of people being pure begins with researchers adopting categories of ethnicity and race and then labelling these categories per the sample sets.{17} However, as noted earlier, the definition of race has changed over time. This is a subject that appears to be far from settled in the U.S., let alone globally, regardless the damage it can do in healthcare.
Conclusion
Though, from a biological perspective, race is now being acknowledged as a social construct, the perceived notion of race still carries with it impacts from a racist past to the present day in terms of healthcare equity.
A formula from nearly 200 years ago is still used for measuring BMI, though its own creator noted that it should not be utilized on an individual basis. Another formula with its inception in the times of slavery—and utilized nefariously to justify slavery—is now insidiously programmed into the spirometer. The formula for diagnosing AKI segregates Black from non-Black.
The very essences of the medical uses of BMI, AKI, and the spirometer are flawed in application. This has real consequences for clinical research, such as poorly designed clinical study protocols that use formulas for BMI or AKI to exclude would-be participants from trials for which they would otherwise be qualified. In the healthcare setting, the real consequences can be with diagnosis and treatment; a formula may deliver a false negative, in that the individual may be sicker than the formula shows, especially in cases of AKI and spirometer usage.
With the examples provided in this review, it is important that those within healthcare and clinical research be vigilant to how the tenants of equitable treatment must be re-evaluated regarding the social realities of race and how to mitigate the disparities that are created from misapplication of outdated concepts tied to race. Further, educators should be aware that strains of racism are still present and embedded in the fabric of healthcare. Healthcare curricula in our educational institutions at all levels need to reflect the most updated concepts regarding what exactly race is, and to teach it as a social construct that impacts the lives of various groups.
It is important that the individual patient be seen as an individual, and not “stereotyped” into a group when it comes to healthcare. Educators should address in class how healthcare disparities arise when different groups are treated differently and homogenously, and how the environments individual patients grow up in account for far more in their health journeys than any superficial difference of “race.” Continuing education is also needed for established professionals to learn about new models for addressing disparities in healthcare and research settings.
To truly bring about change and equity, the formulas and paradigms that have been held for the past 200 years must be deprogrammed, and it is time for healthcare and clinical research to evolve away from stereotyping groups and toward elevating care for individuals.
References
- Daher Y, Austin E, Munter B, Murphy L, Gray K. 2021. The History of Medical Education: A Commentary on Race. Journal of Osteopathic Medicine121(2):163–70. https://doi.org/10.1515/jom-2020-0212
- Washington HA. 2006. Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present. https://www.penguinrandomhouse.com/books/185986/medical-apartheid-by-harriet-a-washington/
- Emanuel EJ, et al. (editors). 2003. Ethical and Regulatory Aspects of Clinical Research: Readings and Commentary. Baltimore: Johns Hopkins University Press. https://www.amazon.com/Ethical-Regulatory-Aspects-Clinical-Research/dp/0801878136
- Stern C. 2021. Why BMI is a Flawed Health Standard, Especially for People of Color. The Washington Post. https://www.washingtonpost.com/lifestyle/wellness/healthy-bmi-obesity-race-/2021/05/04/655390f0-ad0d-11eb-acd3-24b44a57093a_story.html
- Weir CB, Jan A. 2019. BMI Classification Percentile and Cut Off Points. StatPearls.
https://pubmed.ncbi.nlm.nih.gov/31082114/ - Brazier Y. 2021. How Useful is Body Mass Index (BMI)? Medical News Today. https://www.medicalnewstoday.com/articles/255712
- Christine B. 2020. The BMI is Racist and Useless. Here’s How to Measure Health Instead. HuffPost. https://www.huffpost.com/entry/bmi-scale-racist-health_l_5f15a8a8c5b6d14c336a43b0
- Laster M, Shen JI, Norris KC. 2018. Kidney Disease Among African Americans: A Population Perspective. American Journal of Kidney Diseases 72(5):S3–7. https://pubmed.ncbi.nlm.nih.gov/30343720/
- Teo SH, Endre ZH. 2017. Biomarkers in Acute Kidney Injury (AKI). Best Practice & Research Clinical Anaesthesiology31(3):331–44. https://pubmed.ncbi.nlm.nih.gov/29248140/
- Vyas DA, Eisenstein LG, Jones DS. 2020. Hidden in Plain Sight—Reconsidering the Use of Race Correction in Clinical Algorithms. New England Journal of Medicine 383(9):874–82. https://pubmed.ncbi.nlm.nih.gov/32853499/
- Bichell RE, Anthony C. 2021. Kaiser Health News. https://khn.org/news/article/black-kidney-patients-racial-health-disparities/
- Braun L. 2015. Race, Ethnicity, and Lung Function: A Brief History. Canadian Journal of Respiratory Therapy 51(4):99–101. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4631137/
- Lujan HL, DiCarlo SE. 2018. Science Reflects History as Society Influences Science: Brief History of “Race,” “Race Correction,” and the Spirometer. Advances in Physiology Education. https://pubmed.ncbi.nlm.nih.gov/29616572/
- Anderson MA, Malhotra A, Non AL. 2021. Could Routine Race-Adjustment of Spirometers Exacerbate Racial Disparities in COVID-19 Recovery? The Lancet Respiratory Medicine9(2):124–5. https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30571-3/fulltext
- Witzig R. 1996. The Medicalization of Race: Scientific Legitimization of a Flawed Social Construct. Annals of Internal Medicine 125(8):675–9. https://pubmed.ncbi.nlm.nih.gov/8849153/
- Smart A, Bolnick DA, Tutton R. 2017. Health and Genetic Ancestry Testing: Time to Bridge the Gap. BMC Medical Genomics 10(1):1–9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5223458/
- Blell M, Hunter MA. 2019. Direct-to-Consumer Genetic Testing’s Red Herring: “Genetic Ancestry” and Personalized Medicine. Frontiers in Medicine6(48). https://www.frontiersin.org/articles/10.3389/fmed.2019.00048/full

Preethi Sriram, DHSc, MSN, BSN, (SriramPreethi@hotmail.com) is a Clinical Research Professional in Raleigh, N.C.



