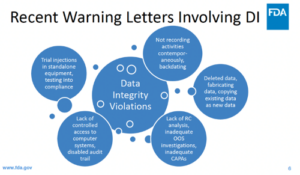
Data integrity issues continue to be uncovered by U.S. Food and Drug Administration (FDA) investigators, leading to a range of regulatory actions. Between 2017 and 2022, FDA issued more than 160 Warning Letters citing data integrity deficiencies,{1} which relate to the completeness, consistency, and accuracy of data.{2} Recent Warning Letters have focused on topics including deleted data, fabricated data, copying existing data as new data, and lack of controlled access to computer systems (see Figure 1).
“These continuing violations reflect the increasing use of technology in clinical research, including digital health approaches that improve patient access,” says Craig Garmendia, PhD, MS, Investigator, International Inspection Cadre, FDA. “These facilitate data gathering so that study results are more representative of the general population. However, challenges remain, including potential lack of understanding of how technologies work. Mistakes can lead to unusable data. We must learn from these to ensure that subjects’ participation in clinical trials yields valuable results.”
Garmendia describes one recent real-world example of issues with electronic data on efficacy and safety in which a principal investigator was given a tablet computer to report the primary efficacy endpoint of a clinical trial. “FDA inspectors noticed a long lag time—sometimes as long as two years—between the data being recorded and [their] submission to the sponsor’s central data base,” notes Garmendia. “The inspectors found that the tablet did not produce an audit trial, so was not compliant with Part 11 of Title 21 of the Code of Federal Regulations (21 CFR Part 11).{3} This meant that changes could have been made to the data, posing a risk to data integrity, with the result that the sponsor had to withdraw its marketing application.”
Figure 1: Recent FDA Warning Letters involving data integrity [from April 2022 presentation]{2}
Garmendia adds that in a second example, a study was designed to measure biometrics using a wearable device. “This device was worn for 24 hours, then the subject returned to the study site to download the data. FDA inspectors found that the device did not have an alarm to detect removal by the patient. As a result, there was no way to know whether the device had been worn for the full period, invalidating the data. In another case, an unvalidated algorithm was used to analyze primary efficacy data, leading to endpoint data not being reliably detected. The resulting data [were] not acceptable as part of a marketing application.”
Two Steps Forward, One Step Back: Getting Ahead of Tech-Related Data Integrity Challenges
Join Craig at ACRP 2024 [May 3 – 6; Anaheim, Calif.], as he provides insight into electronic data on efficacy and safety and some real-world examples of questionable validity that the FDA has seen recently. View complete schedule.

“The major learning from these examples is the need for sponsors to carry out a thorough risk assessment on their technology, making sure that it is validated and appropriate for clinical, scientific, and regulatory needs,” concludes Garmendia. “Sponsors should keep in mind that FDA review of study protocols is at a high level, with details such as technology validation examined at a later stage. While health technologies are powerful tools, these must be used appropriately to ensure data integrity. This will support the mission of ensuring that only safe and effective products reach the market, helping protect public health.”
References
- https://www.sciencedirect.com/science/article/abs/pii/S0378517322010584?via%3Dihub
- https://www.fda.gov/media/165535/download
- https://www.fda.gov/regulatory-information/search-fda-guidance-documents/part-11-electronic-records-electronic-signatures-scope-and-application
Edited by Jill Dawson