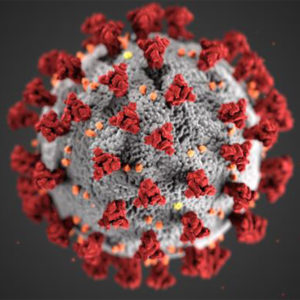
Researchers are using computer models to simulate COVID-19 infections on a cellular level—the basic structural level of the human body. The models allow for virtual trials of drugs and vaccines, opening the possibility of pre-assessment for drug and vaccine efficacy against the virus.
The research team at the University of Waterloo includes Anita Layton, a professor of applied mathematics, and Mehrshad Sadria, an applied mathematics doctoral student.
The team uses in silico experiments to replicate how the human immune system deals with the COVID-19 virus. In silico refers to trials situated in the silicon of computer chips, as opposed to in vitro or in vivo experiments, situated in test tubes or directly in living organisms.
“It’s not that in silico trials should replace clinical trials,” Layton says. “A model is a simplification, but it can help us whittle down the drugs for clinical trials. Clinical trials are expensive and can cost human lives. Using models helps narrow the drug candidates to the ones that are best for safety and efficacy.”
The researchers, among the first to be working on these models, were able to capture the results of different treatments that were used on COVID-19 patients in clinical trials. They say that their results, published in the journal Viruses, are remarkably consistent with live data on COVID-19 infections and treatments.
One example of a treatment used in the model was Remdesivir, a drug that was used in the World Health Organization’s global SOLIDARITY trials. The simulated model and the live trial both showed the drug to be biologically effective but clinically questionable, unless administered shortly after viral infection.
The model might also work for current and future variants of concern. The researchers anticipate the virus will continue to undergo mutation, which could precipitate new waves of infection.
“As we learn more about different variants of concern, we can change the model’s structure or parameters to simulate the interaction between the immune system and the variants,” Sadria says. “[Then we can] predict if we should apply the same treatments or even how the vaccines might work, as well.”
Edited by Gary Cramer