Clinical Researcher—August 2023 (Volume 37, Issue 4)
PEER REVIEWED
Sherajum Monira, MS; Martha Toral
Digital medicine, often referred to as mobile health, is a rapidly emerging field that relies on evidence-based, state-of-the-art technologies in contrast to traditional medicine to transform the way healthcare is delivered.{1} Powered by high-quality hardware and software, this ground-breaking technology collects and tracks health data that can be used to manage critical health conditions. It facilitates sophisticated and accessible tools for patients and healthcare practitioners to address a wide range of illnesses through high-quality, safe, and effective measures and data-driven interventions.
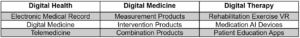
Measurement, intervention, and combination goods are the three primary categories of digital medicine products, as shown in Table 1.{1} Numerous digital medicine products can be used in healthcare—for example, smart insulin pens that monitor insulin levels, pills with cameras built in for detecting colon cancer, blood sugar monitoring wearable sensors, artificial intelligence (AI) that can look for suspected cancer indications during a colonoscopy, smartwatch sensors that can record heart rhythm, and early detection of cancer.{2,3}
Table 1: Distinction Between Digital Health, Digital Medicine, and Digital Therapeutics
Digital medicine represents a paradigm change in oncology research by harnessing technological breakthroughs to address the constraints of traditional clinical trial procedures. Researchers may collect huge amounts of patient-generated health data by adding digital tools into the clinical trial process, providing for a more comprehensive assessment of illness development, treatment response, and potential adverse events. Furthermore, digital medicine allows for continuous remote monitoring, removing geographic obstacles, improving patient convenience and accessibility, and fostering medical research and innovation.
This article navigates into the recent development and background of digital medicine in the field of oncology trials and explores its future potential and advantages. Further, it depicts the key challenges such as privacy, security, and technical instructions which need to be addressed to unlock its true potential.
Background
In 2020, an estimated 19.3 million new cancer cases and 10 million cancer deaths were reported worldwide. Further, in 2040, there are expected to be 28.4 million new cancers, almost a 50% rise from 2020.{4} This trend is extremely concerning and highlights the growing global burden of cancer. Cancer care faces major hurdles due to a lack of medical resources and an uneven distribution of medical care levels. The encouraging aspect is that digital medicine includes a wide range of cutting-edge technology and applications like machine learning, AI, and cloud computing to provide promising solutions to cancer patients.
Although digital medicine is still in its early stages, it has the potential to transform cancer care in a variety of ways, such as identifying diseases early, providing more effective treatments, and enhancing patient outcomes by enabling more precise, personalized, and data-driven approaches. Healthcare workers may improve patient outcomes and minimize the burden of cancer on individuals and healthcare systems by leveraging the ground-breaking power of digital technologies.
The Merits of Digital Medicine
The use of digital medicine in oncology clinical trials has brought many benefits to studies, including applicability, improved cost-effectiveness, patient benefits, increased accuracy of real-time data collection, and personalized and adaptive treatment plans.{1} The encouraging applicability and flexibility of digital medicine are allowing this technology to be integrated into oncology studies.
Another aspect of digital medicine that is attractive to researchers is the potential to decrease healthcare costs as well as the time a patient spends accessing healthcare.{1} One example of individuals spending less time receiving medical care is through teledermoscopy. In Australia, a study showed the use of teledermoscopy in the diagnosis or treatment of skin cancer resulted in a decreased clinical resolution by 26 days. However, the cost was $54.64 more than the use of non-digital medicine.{5} In this particular case, one can argue that, although the cost of treatment may be higher, the significant time reduction in resolution may also be cost-effective if other factors are reviewed. For instance, the increased lag time in treatment for a patient with difficulties traveling to the clinic could increase costs for an individual not receiving the proper care in a timely manner.
Digital medicine can be utilized to not only lower cost, decrease time, and increase accessibility to those in rural areas or individuals facing challenges traveling to the clinic, but also to increase recruitment and help close the equity gap in healthcare. Digital medicine also has the potential to improve the quality of care for a patient and increase the efficiency of patient enrollment in oncology trials.{6}
Technological devices containing sensors to monitor a patient’s physiological activities can improve the treatment and early diagnosis of a disease.{1} This real-time information occurs while the patient is at home or conducting their daily activities, and can be used to further monitor oncology clinical trial patients while receiving treatment. The additional and abundant amount of information can result in valuable data for a researcher, potentially increasing the safety profile and improving quality control.{1}
Other ways oncology clinical trials have been able to take advantage of digital medicine is through the use of AI and natural language processing.{1} These digital medicines were shown to have equal or superior capabilities when compared to manual screening in patent enrollment in cancer clinical trials.{6} A meta-data analysis of information from articles that identified using AI for patient enrollment in oncology trials had promising findings. The analysis revealed that out of the 19 datasets used, 18 had an 80% or better accuracy, sensitivity, and specificity than manual screening for patient enrollment in oncology trials.{6}
If digital medicine is able to facilitate the screening and enrollment process in cancer clinical trials, this can move clinical trials at a faster pace, ensuring adequate and eligible patients are enrolled. This technology can also be used at a wider scale by including information from patients in numerous hospitals and other facilities across the United States or globally to identify clinical trials a patent would qualify for. This capability would drastically increase enrollment and improve the dire enrollment rates that currently exist in oncology trials, where the enrollment of cancer patients is less than 5% and almost 20% of oncology trials end early due to enrollment issues.{6}
The many advantages offered by the variety of digital medicines currently being developed and those currently used bring a bright prospective future to the advancement of research, diagnosis, and treatment of cancer.
Applications of Digital Medicine in Oncology Trials
Cancer prevention, screening, therapy management, and follow-up can all benefit from the use of digital medicine. The collected data can also be used for scientific study, clinical quality control, and other objectives, which will aid in the resolution of current tumor-related medical issues.
Cancer Prevention
Cancer prevention can benefit tremendously from digital medicine. A plethora of digital medicine resources, such as sun protective behaviors and tumor prevention via mobile phone applications, have been developed and applied to encourage health behavior change. Recently, the relationship between wearing an ultraviolet (UV) radiation monitoring device and UV exposure discovered that parental and child outdoor activity and sunscreen use time varied considerably after wearing the monitoring device, which is crucial for skin cancer prevention.{7}
Numerous research efforts reveal that obesity plays a significant role in most common cancers such as breast cancer, colorectal cancer, endometrial cancer, renal cell cancer, and esophageal cancer. Thanks to digital medicine, recent mobile apps can facilitate the shaping of individuals’ approaches to cancer prevention. Patients are presently adopting mobile health modalities for managing cancer caused by obesity, since they offer tracking and monitoring, give dietary and exercise recommendations, provide encouragement for medication adherence, allow for distant treatment, and supply individualized treatment.{8} Weight loss and a decline in body mass index were found to be strongly correlated in a recent meta-analysis looking at the impact of mobile app interventions.{9}
Cancer Screening
Digital medicine has potential for improving tumor screening and diagnosis by utilizing big data technology and machine learning algorithms to detect cancer at an earlier stage. A study using a web-based chatbot, for example, found that women’s cancer risk may be predicted in advance using collected information about a patient’s family history of cancer and following recognized guidelines.{10} This scalable solution can successfully assess cancer risk, detect adverse events or recurrence earlier, engage patients in educational material, and pave the way for preventive genetic testing, which could lead to better patient outcomes and more efficient cancer therapy.
By identifying high-risk patients ahead of time, medical practitioners can provide tailored and focused care during visits to them. The chatbot assessed one-quarter of the subjects who met the USA National Comprehensive Cancer Network genetic testing criteria. Furthermore, digital biomarkers can be generated by digital medicine products for early-stage cancer detection. Sensors detect or algorithms infer digital biomarkers. A noninvasive sensor will be able to monitor specific tumor targets in the future.
Cancer Treatment
The use of smartphone mobile games for chemotherapy self-management in patients with breast cancer is an intriguing and promising breakthrough in cancer care. A related study’s findings are positive, indicating that web-based self-management mobile games, when compared to traditional education approaches, have the potential to increase patient education, drug compliance, psychological status, and quality of life, and to lessen physical side effects.{11}
Meanwhile, clinical decision support systems (CDSS) are computer-based technologies that can assist healthcare providers in making efficient and educated cancer treatment decisions based on patient data. For example, based on a patient’s cancer type, stage, and genomic profile, CDSS can recommend the best chemotherapy plan. Recent findings suggest that higher level CDSSs that employ automated clinical guidelines, AI, data mining, and statistical approaches can result in considerable improvements in process outcomes and guideline adherence.{12}
Privacy and Security Challenges
Privacy and security issues are major concerns in digital medicine when considering data sharing and the use of data-sharing platforms. Although the sharing of de-identified data of a patient is an important tool for researchers, the National Institutes of Health (NIH) requires some researchers to make their data available to other researchers through an NIH database, and this can create privacy and security issues.{13} The risk of re-identification is present as identifiable markers in a dataset can be used. The use of digital medicine and the transfer of subject information at a faster pace, and at times in real-time, would increase these risks and certain provisions would need to be added to decrease these dangers.
When considering databases such as the Personal Genome Project (PGP), which is a significant scientific achievement, one must consider their potential threats to privacy. The profiles in the PGP database were connected to names and contact information by using the database’s demographics and comparing them to information found in public records.{13} Another example is the Project Data Sphere platform, which is an open-access data-sharing database entirely built on oncology clinical trial data.{14} Currently, the database contains raw deidentified late-phase oncology clinical trial information from 120,000 patients including more than 20 tumor types.{14}
While the benefits of such databases are significant, one must wonder if they outweigh the risks. A large benefit to these data-sharing platforms comes from the potential to collaborate with numerous researchers nationally and internationally. Another advantage is that a researcher has the ability to answer research questions in a short time, increasing their efficiency. Additionally, these data can serve as surrogate endpoints and assist with the selection of subgroups in clinical trials investigating new oncology therapies.{15}
As another example, since it is a tool that is seen as highly advantageous, there isn’t much scrutiny given to those who request access to Data Share. This platform prides itself on its open-access model for the reasons mentioned above, even though it provides the least amount of scrutiny for its users. Once an individual is given access, they have full access to the copious amounts of late-phase oncology information, which can result in potential misuse of these data.
Although the capability exists through these databases to further cancer research and bring forth novel therapies in a more efficient way, for example, by informing researchers on the dose adjustments for chemotherapy patients or leading to changes in national guidelines,{15} the patient’s safety, including aspects related to their privacy and confidentiality, should come before any potential benefit. To limit these risks, one would need to perform a well-developed balancing act by restricting specific information yet providing accurate data.
Innovation of Future Treatment
The future of digital medicine holds a lot of potential for cancer treatment. Using cutting-edge digital technologies, doctors and researchers can develop more efficient, personalized, and patient-centered cancer treatments that improve patient outcomes and quality of life. Here are some potential digital medical advancements for future cancer treatment.
Artificial Intelligence
Scientists supported by the National Cancer Institute are already using AI to improve cancer detection in cervical and prostate cancer. They have also developed AI applications for improving cancer screening, diagnosis accuracy, and cancer surveillance.
AI algorithms can swiftly assess massive volumes of patient data and assist clinicians in making correct clinical and therapy decisions. Others use it to evaluate imaging data and electronic health records to personalize radiation doses for patients. The U.S. Food and Drug Administration (FDA) has approved the first AI-based software to analyze images quickly and help radiologists detect breast cancer in screening mammography.{16}
These are merely illustrative examples. AI could truly improve cancer care in the future by developing novel cancer medicines or forecasting a patient’s risk.
Advancing Smart Technology
Wearable technology is revolutionizing cancer treatment with the aid of real-world and real-time data from patients. Wearables have the potential to significantly improve cancer patients’ ability to control their condition. Patients, for example, frequently feel nausea and other common side effects because of chemotherapy treatments and the illness itself; this condition is easily cured with a simple workout plan. Wearables linked to smartphone apps for data logging can easily track this. Also, wearable sensors and smartphone apps can be used to collect digital biomarkers.
iPhones are also low-cost and user-friendly medical tools for tumor detection. For instance, the FDA recently approved the Butterfly network’s novel ultrasound-based imaging system, which links to an iPhone.{17} This AI-based app is capable of scanning the full body from head to toe, and works in tandem with hardware to help experts evaluate diagnoses and deliver improved treatments.
Conclusion
Oncology clinical trials are being transformed by digital medicine, which uses technology to enhance patient interaction, monitoring, and treatment plans. We can hasten the development of novel medicines, improve patient care, and eventually make major progress in the fight against cancer by embracing digital technologies and data-driven methodologies.
The key aspects of cancer treatment are early detection and personalized care, and they have never seemed more feasible than they do now, thanks to breakthroughs showing promise in oncology clinical trials made possible by wearable devices, smartphone apps, AI, and machine learning algorithms. Data from oncology clinical trials are proving the potential for digital medicine technology to offer more inexpensive and less intrusive cancer management solutions, and the development of a comprehensive and successful cancer-fighting strategy more likely by the day in the digital era.
References
- Ge H, Li L, Zhang D, Ma F. 2022. Applications of digital Medicine in oncology: Prospects and challenges. Cancer Innovation. https://onlinelibrary.wiley.com/doi/full/10.1002/cai2.37
- Aungst T. 2021. What’s the Difference Between Digital Health, Digital Medicine, and Digital Therapeutics? GoodRx Health. https://www.goodrx.com/healthcare-access/telehealth/digital-therapeutics-vs-digital-medicine-vs-digital-health
- Smart Watches Hold Promises to Detect Disease and Improve Health. 2022. University Hospitals. https://www.uhhospitals.org/blog/articles/2022/09/smart-watches-hold-promise-to-detect-disease-and-improve-health
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. 2021. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. National Library of Medicine. https://pubmed.ncbi.nlm.nih.gov/33538338
- Snoswell CL, Caffery LJ, Whitty JA, Soyer HP, Gordon LG. 2018. Cost-Effectiveness of Skin Cancer Referral and Consultation Using Teledermoscopy in Australia. JAMA Dermatology 154(6):694–700. https://doi.org/10.1001/jamadermatol.2018.0855
- Chow R, Midroni J, Kaur J, Boldt G, Liu G, Eng L, Liu F-F, Haibe-Kains B, Lock M, Raman S. 2023. Use of Artificial Intelligence for Cancer Clinical Trial Enrollment: A Systematic Review and Meta-Analysis. JNCI: Journal of the National Cancer Institute. https://doi.org/10.1093/jnci/djad013.
- Parsons BG, et al. 2021. Reactivity to UV Radiation Exposure Monitoring Using Personal Exposure Devices for Skin Cancer Prevention: Longitudinal Observational Study. JMIR Mhealth Uhealth. https://mhealth.jmir.org/2021/9/e29694
- Panayi ND, Mars MM, Burd R. 2013. The promise of digital (mobile) health in cancer prevention and treatment. Future Medicine. https://www.futuremedicine.com/doi/10.2217/fon.13.42
- Islam M, Poly TN, Walther BA, Li Y-C. 2020. Use of Mobile Phone App Interventions to Promote Weight Loss: Meta-Analysis. JMIR Mhealth Uhealth. https://mhealth.jmir.org/2020/7/e17039
- Shivani N, et al. 2021. Hereditary Cancer Risk Using a Genetic Chatbot Before Routine Care Visits. Obstetrics & Gynecology. https://journals.lww.com/greenjournal/Fulltext/2021/12000/Hereditary_Cancer_Risk_Using_a_Genetic_Chatbot.7.aspx
- Kim HJ, Kim SM, Shin H, Jang J-S, Kim YI, Han DH. 2018. A Mobile Game for Patients with Breast Cancer for Chemotherapy Self-Management and Quality-of-Life Improvement: Randomized Controlled Trial. JMIR Mhealth Uhealth. https://www.jmir.org/2018/10/e273/
- Klarenbeek SE, et al. 2020. The Effect of Higher Level Computerized Clinical Decision Support Systems on Oncology Care: A Systematic Review. National Library of Medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7226340/
- Filkins BL, Kim JY, Roberts B, Armstrong W, Miller MA, Hultner ML, Castillo AP, Ducom J-C, Topol EJ, Steinhub SR. 2016. Privacy and Security in the Era of Digital Health: What Should Translational Researchers Know and Do about It? Am J Transl Res 8(3):1560–80.
- Project Data Sphere. www.projectdatasphere.org
- Green AK, Reeder-Hayes KE, Corty RW, Basch E, Milowsky MI, Dusetzina SB, Bennett AV, Wood WA. 2015. The Project Data Sphere Initiative: Accelerating Cancer Research by Sharing Data. The Oncologist 20(5):464-e20. https://doi.org/10.1634/theoncologist.2014-0431
- Artificial Intelligence – Opportunities in Cancer Research. 2020. National Cancer Institute. https://www.cancer.gov/research/areas/diagnosis/artificial-intelligence
- Zukova M. 2020. Digital health and oncology: A growing world of personalization, diagnosis, and prognosis. Healthcare IT News. https://www.healthcareitnews.com/news/emea/digital-health-and-oncology-growing-world-personalisation-diagnosis-and-prognosis

Sherajum Monira, MS (sherajum.monira@sjsu.edu) recently earned her master’s degree in Medical Product Development Management at San Jose State University, San Jose, Calif.
Martha Toral is a Global Study Associate with Treadwell Therapeutics Inc. and a graduate student in Medical Product Development Management at San Jose State University, San Jose, Calif.



